Abstract
Background
The survival of childhood acute lymphoblastic leukemia (ALL) has improved significantly over the last decades, with recently reported overall survival rates in Europe of up to 85% in children (<14 years) and 62% in adolescents (15-19 years) (Trama, Lancet Oncol 2016). The increased number of long-term survivors has made the management of side effects an increasingly important issue in pediatric oncology. In this context, the impact on fertility caused by widely employed ALL treatments such as alkylating agents, cranial radiotherapy, total body irradiation and orchiectomy has been an emerging concern over the last years. The aim of this study was to assess fertility among long-term childhood ALL survivors.
Methods
Between 2012 and 2017, a follow-up study was performed among childhood ALL (and acute lymphoblastic lymphoma) survivors enrolled between 1971 and 1998 in EORTC studies (58741, 58831/2, 58881) in France and Belgium. Patients <18 years (yrs) at diagnosis and ≥18 yrs at the time of the follow-up were eligible to fill out a questionnaire that included information about their fertility. The following fertility-related outcomes were evaluated: having menstrual cycles for females, intention to have children, having children, use of reproductive techniques to become pregnant and occurrence of negative pregnancy outcomes (miscarriage, medical abortion, birth defects), separately for males and females.
Results
Out of 1429 eligible patients, 502 (35%) filled out the questionnaire, 862 (60%) were lost to follow-up, and 65 (5%) refused to participate. Disease characteristics and relapse occurrence within one yr after diagnosis were comparable between these 3 groups.
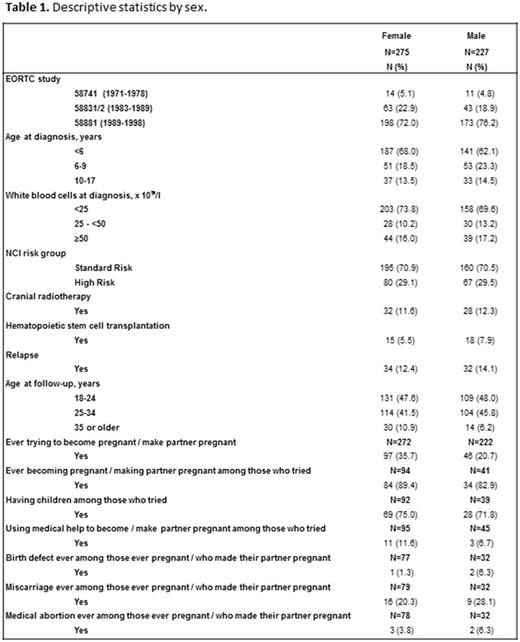
Among respondents (275 females, 227 males), approximately 14% were aged 10-17 yrs at diagnosis and almost 30% belonged to the NCI high risk group (Table 1). Approximately 12% received cranial radiotherapy and 6% of females and 8% of males underwent hematopoietic stem cell transplantation. Relapse occurred in 12% and 14% of females and males, respectively. The median time between the diagnosis and the socioeconomic evaluation was 20 yrs (range: 13-42). The median age at follow-up was 25 yrs (range: 18-53).
All but 6 females had ever had menstrual cycles. At the time of the fertility evaluation, 93% out of females younger than 45 yrs of age (N=270) either had menstrual cycles, were pregnant, gave breast feeding or continuously used contraceptives. Among females who had tried to become pregnant, 89% had been pregnant, 75% had children and 12% used medical help to become pregnant. One fifth of the ever pregnant females had ever had a miscarriage. The incidences of other negative pregnancy outcomes (e.g. birth defect, medical abortion) were low.
The average number of children females had was 0.36 (95% CI: 0.27-0.44). The expected number of children in a population with the same distribution of country, age, and yr of birth of the mothers based on national population registries was 0.55. However, as 52% of the females had a bachelor or master degree and only 3% had no secondary school diploma, this difference could possibly be explained by an overrepresentation of females with a high level of education in our sample.
Among males who had tried to have children, 83% made their partner pregnant, 72% had children and 7% used medical help to make their partner pregnant. The incidence of negative pregnancy outcomes other than miscarriage was low.
Conclusions
In this first disease-specific European cohort study, we evaluated fertility among adult survivors of childhood ALL enrolled in EORTC trials, with a median time from the diagnosis of 20 yrs.
Most survivors who tried to have children, succeeded (75% of females, 72% of males). However, the average number of children per female seemed to be lower than in the general population. The incidences of birth defects, and medical abortions were low, both among female survivors and the partners of the male survivors.
Despite the large number of potentially eligible patients, we could evaluate only 35% of long-term survivors. We were unable to study the effect of specific treatment exposures due to the large variety of treatments that patients received, the association between some treatments (protocol dependent) and age at the fertility evaluation, and the need to stratify the analyses by sex. Improvements in the follow-up of childhood cancer survivors are needed for a better evaluation of the long-term outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal